We need good energy!
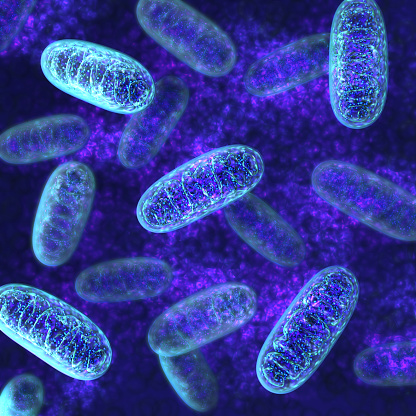
Everything we do requires energy – running, walking, sleeping, thinking, eating, and yes, even sleeping. We get that from our food, but there is a tiny miracle happening in all of us right now which converts our food into energy, and the machinery which performs that critical job is called Mitochondria.
These are tiny organelles found in each of our cells that play a starring role in converting nutrients into the body’s primary fuel source, which is called adenosine triphosphate (ATP). For something so tiny they have a mighty job. This all happens via a biochemical pathway called the electron transport chain.
How damage to Mitochondria leads to illness
Mitochondria are prone to damage, and that loss can lead to illness. Mitochondrial dysfunction is associated with conditions such as:
- Autism
- Asperger’s syndrome
- Chronic fatigue syndrome
- Fibromyalgia
- Parkinson’s
- Alzheimer’s
- Depression
- Schizophrenia
- Bipolar disease
- Lupus and
- Diabetes
How do Mitochondria get damaged?
It is DNA damage and reactive oxygen species (ROS) generation (think free radical damage and oxidative stress) in mitochondria that cause mitochondrial damage. ROS are unfortunate byproducts of cellular metabolism, and an increase in ROS means aging and neurodegeneration over time.
Mitochondrial dysfunction can be inherited from the mother via the mitochondrial genetic mutations they carry. Mothers carry the genes that contribute mitochondria to their children. Mitochondrial dysfunction can also be acquired, and this is due to environmental and pharmaceutical toxin exposure.
Today’s world of chemicals and toxins makes it is easy to understand that damage to mitochondria is frequent and needs to be addressed. Lastly, mitochondrial damage happens as we age. Preserving mitochondrial function can help increase longevity.
What you can do to correct Mitochondrial dysfunction
There are some proven ways to improve existing mitochondrial function and create new healthy mitochondria.
The body is thought to require exposure to a stressor, a challenge to the system. Exercise, a ketogenic diet, intermittent fasting, exposure to cold and hot extremes are all considered stressors that the body responds to by regenerating and improving mitochondrial function.
Specific nutrient supplementation has also been found to assist in the restoration of healthy mitochondrial function and the biogenesis of mitochondria.
The power of exercise
Exercise improves mitochondrial function. The key is endurance-based exercise. Walking does not count. Increasing your heart rate with activities such as running, cycling or swimming long distances you can stimulate the production of more mitochondria to create more ATP.
Ketones
When you eat a high fat and low carbohydrate diet you are creating a scenario where the body perceives it is in starvation mode. The liver relies on using fat from our food or from our bodies, rather than glucose to create fuel for the body and brain.
Ketone bodies are produced in the liver by fatty acids and used for energy production, and ketones have been found to be a more efficient fuel than glucose. They can cross the blood-brain barrier to fuel the brain, which requires 20 percent of our daily energy requirements. Ketones have been found to increase the number of mitochondria and reduce the production of ROS, which depletes mitochondrial function.
A quick note here: Ketogenic diets are not for everybody and should not be undertaken without the supervision of a trained health professional.
Cell protection with fasting
Intermittent fasting or calorie restriction helps protect mitochondria from damage and reduces ROS production. Reliance on fat (as discussed above) for energy production during periods of calorie restriction causes cells to switch into survival mode and remove unhealthy mitochondria and replace them with healthy ones. This means less free radical production.
Exposure to extreme hot and cold temperatures
We know stressors are what help initiate mitochondrial repair and production and hot or cold extremes do just that. Exposing the body to elevated temperatures via exercising, sauna and steam rooms, activate genes that optimise heat shock proteins inside cells, leading to an increase in mitochondrial production. As with heat, habitually exposing yourself to unusually cold temperatures enables heat production in the body. More heat production or cold thermogenesis, due to activation of brown adipose fat tissue, causes more mitochondria and ATP to be made.
Nutrients – proper nutrition for your cells
Particular nutrients have been studied to look into their role in improving mitochondrial function:
L-Carnitine
Carnitine deficiency is associated with mitochondrial dysfunction, and L-carnitine is essential in the restoration of mitochondrial function as it is a fatty acid transporter in the mitochondria that supports energy production.
Alpha lipoic acid
Alpha-lipoic acid is an antioxidant that restores mitochondrial glutathione levels (an important antioxidant) that reduce ROS formation and increase electron transport function, resulting in more ATP creation.
Coenzyme Q10
Coenzyme Q10 is a crucial cofactor for the electron transport chain and antioxidant that when supplemented at high dose helps restore mitochondrial function and increase energy production.
 This article was written by Naturopath, Susan Hunter,
This article was written by Naturopath, Susan Hunter,
B.HSc (Naturopathy), BA (Psych)
You can find out more about Susan at The Healthful Clinic
For more on Mitochondria see our article:
When Fatigue Gets You Down: A Guide to Understanding Mitochondrial Disease
References
Barbato, D.L. and Aquilano, K., 2016. Feast and famine: Adipose tissue adaptations for healthy aging. Ageing research reviews, 28, pp.85-93.
Cohen, B.H. and Gold, D.R., 2001. Mitochondrial cytopathy in adults: what we know so far. Cleveland Clinic journal of medicine, 68(7), pp.625-642.
Filler, K., Lyon, D., Bennett, J., McCain, N., Elswick, R., Lukkahatai, N. and Saligan, L.N., 2014. Association of mitochondrial dysfunction and fatigue: a review of the literature. BBA clinical, 1, pp.12-23.
Frye, R.E. and Rossignol, D.A., 2011. Mitochondrial dysfunction can connect the diverse medical symptoms associated with autism spectrum disorders.
Iversen, N., Krustrup, P., Rasmussen, H.N., Rasmussen, U.F., Saltin, B. and Pilegaard, H., 2011. Mitochondrial biogenesis and angiogenesis in skeletal muscle of the elderly. Experimental gerontology, 46(8), pp.670-678.
Jornayvaz, F.R. and Shulman, G.I., 2010. Regulation of mitochondrial biogenesis. Essays in biochemistry, 47, pp.69-84.
Maalouf, M., Sullivan, P.G., Davis, L., Kim, D.Y. and Rho, J.M., 2007. Ketones inhibit mitochondrial production of reactive oxygen species production following glutamate excitotoxicity by increasing NADH oxidation. Neuroscience, 145(1), pp.256-264.
Nicolson, G.L., 2014. Mitochondrial dysfunction and chronic disease: treatment with natural supplements. Integrative Medicine: A Clinician’s Journal, 13(4), p.35.
Siddiqui, M.F., Elwell, C. and Johnson, M.H., 2016. Mitochondrial Dysfunction in Autism Spectrum Disorders. Autism-open access, 6(5).