In analysing Childhood Sleep patterns, children who sleep less have been shown to be prone to a higher body mass index (BMI), and increased anxiety or low self-esteem.
Paradoxically, anxiety and low self-esteem may affect sleep duration and predict increased BMI, according to a recent cross-sectional study.
Spanish researchers analysed the sleep patterns of 291 schoolchildren aged around 9 years old. Using BMI measurements, anxiety and depressions scales, and parent interviews, they aimed to establish how anxiety, low self-esteem and less sleep interact with an increase in children’s weight.
The group’s average sleep time was 9 hours and 50 minutes.
Childhood Sleep Study Results
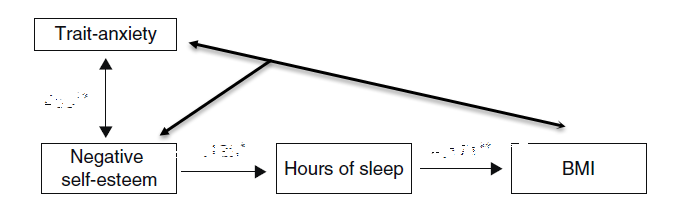
Data analysis showed that high-trait anxiety (anxiety characteristic to their own personality or traits) and negative self-esteem both caused and resulted in an increased BMI.
The researchers observed a cycle – ‘as self-esteem is associated with a reduction of sleep duration that may further promote overweight, while overweight leads to an increase in negative self-esteem.’
The authors summarised that ‘One of the main inferences that could be drawn from this study has to do with preventing childhood overweight. Ensuring proper sleep duration may be a key element in prevention, and in some cases, this could entail the management of emotional states like anxiety or low self-esteem.’
Adapted from: Amigo-Vazquez I, Busto-Zapico R, Pena-Suarez E, et al. [the influence of sleep and emotional states on childhood body mass index]. An Pediatr (Barc). 2015;82(2):83-8.
Childhood Sleep Education and Behaviour Strategies Benefit ADHD Symptoms
A recent randomised controlled trial found ADHD symptom severity was improved with sleep hygiene practices and standardised behavioural strategies.
This Australian study involved 244 children with ADHD aged 2-12 years.
Psychologists and trainee paediatricians, with no prior specialised training in paediatric sleep management, conducted consultations with parents assessing childhood sleep problems, obtaining parent goals and providing information on normal sleep, sleep cycles, sleep cues, and sleep hygiene practices.
These hygiene strategies included:
- a set bedtime
- set routines
- media-free bedrooms and
- avoiding caffeine after 3 pm
Additionally, they set behavioural plans, which included the following:
- ignoring protests and rewarding compliance with bedtime routines
- temporarily setting bedtime later and gradually bringing it forward, while keeping a preset time in the morning to wake the child.
- visual imagery and relaxation techniques for anxiety-related insomnia.
After three and six months, data collection showed a significant reduction in ADHD symptom severity, with children having fewer moderate-severe sleep problems. Approximately 30-50% of the ADHD symptom reduction was due to improved sleep.
They also found improved performance, behaviour and quality of life at school and home, including improved working memory.
The authors concluded that ‘Effects are comparable to those seen with intensive behavioural interventions targeting ADHD symptoms, more wide-reaching than those reported in studies of melatonin, and importantly seem to be sustained over six months. These findings suggest that clinical management of childhood sleep symptoms can reap benefits for the considerable number of children with ADHD who have moderate-severe behavioural sleep problems.’
Mindd Practitioners are trained in the many aspects of Childhood Sleep disturbances to find an Integrative/Functional Medicine Practitioner see our Directory
References
Adapted from: Amigo-Vazquez I, Busto-Zapico R, Pena-Suarez E, et al. [the influence of sleep and emotional states on childhood body mass index]. An Pediatr (Barc). 2015;82(2):83-8.
Hiscock H, Sciberras E, Mensah F, et al. Impact of a behavioural sleep intervention on symptoms and sleep in children with attention deficit hyperactivity disorder, and parental mental health: Randomised controlled trial. BMJ. 2015; doi: 10.1136/bmj.h68.
https://www.bmj.com/content/350/bmj.h68




