For the past few years, the topics of mental health, emotional health and psychological well-being have received some much-needed attention. The Gut-Brain axis is now more relevant than ever.
Emotional Health is Now Front and Center
What was once an area only discussed in the seclusion of a medical appointment, counselling session or support group, emotional health is now a mainstream aspect of our total health and wellbeing. Health blogs, scientific journals and medical conferences are teeming with advice and new research on how to support this fundamental facet of our health.
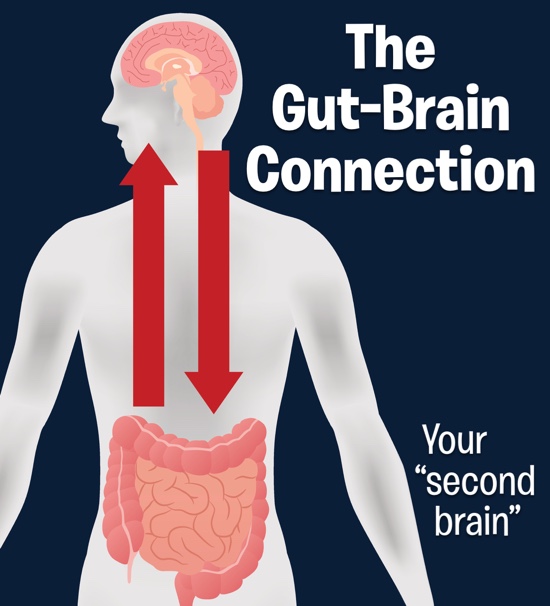
One area of integrative medicine gaining momentum in mental health research is the Gut-Brain Axis. This axis involves chemical signals that occur between your gastrointestinal tract and your nervous system. Studies are showing the intestinal microbiota are particularly influential here, communicating with the brain via several physiological pathways. In the future, it’s possible that many mental health conditions will be treated via amendment of our intestinal microbial populations.
What is the Mechanism of the Gut-Brain Axis?
In medical science research, disease correlations are often found between a specific environmental factor (e.g., diet, lifestyle, medication, pollutant) and a resulting condition or disease state. Correlations are interesting to researchers and the general public alike, but correlations do not prove causation. What is required to prove causation is a cellular mechanism, the discovery of a molecular event that ultimately links a specific environmental factor with causing a condition.
 Does a mechanism exist between the gut microbiome having an influence on brain health? The science for this is very strong, and three mechanisms are receiving a lot of attention:
Does a mechanism exist between the gut microbiome having an influence on brain health? The science for this is very strong, and three mechanisms are receiving a lot of attention:
- The immune mechanism. Microbial populations can cause immune activation directly at the gut mucosal surface membranes. This is especially the case when microbes are pathogenic (disease-causing) members of the microbiome. The enhanced inflammatory response in the gut leads to stimulation of the peripheral immune system. This immune stimulation is able to stimulate specific neurons (nerves) associated with serotonin, a neurotransmitter implicated in many behavioural and emotional health disorders.
- The vagus nerve mechanism. The Gut-Brain Axis is a two-way communication network between your central nervous system (which includes your brain and spinal cord) and your enteric nervous system (a nerve network in your gut). Essentially, this anatomical link establishes a direct, physical connection between the emotional centres of the brain and intestinal function. Studies are revealing that the gut microbiota may signal the brain via nerves, hormones, immune responses and antibodies.
- The bacterial waste product mechanism. Funnily enough, the link between gut and brain health is not new. Just over 100 years ago, patients with depression, anxiety and psychosis were ‘purged’ of their imbalanced state of mind with colonic irrigation and abdominal surgeries. The idea was that poisons originating in the gut were the root cause of these mental health issues. These days, modern medicine has identified these toxins as metabolic by-products (wastes) of certain bacterial populations. Many of these less favourable gut microbes produce neuroactive compounds (including neurotransmitters such as serotonin, melatonin, histamine, acetylcholine and gamma amino butyric acid, GABA) that directly influence brain activity.
Mental Health Conditions Associated With Poor Gut Health
The composition of the gut microbiome is believed to influence the brain in the following conditions:
• Autism
• Anxiety
• Bi-polar
• Depression
• Insomnia
• Schizophrenia
• Poor concentration, aggression, temper and difficulty relaxing
• Overwhelming sense of tension and pressure
• A vast array of other behavioural issues, such as procrastination, teeth grinding and restlessness to name a few.
Five Tips for Supporting Mental Health, Through Your Microbiome
- Avoid the overuse of antibiotics. Thankfully, this message is becoming louder in mainstream medicine. The overuse of antibiotics is one of the main methods of disrupting and destroying a healthy balance of good bacteria in the gut. Only use antibiotics when absolutely necessary, if there is no other alternative.
- Stress management. Everyone finds different life matters stressful, and some people do not find traditional ‘de-stressing’ activities effective. Firstly, identify what causes you the most stress on a daily basis, and speak to a supportive person about ways you can try to manage this. A prolonged stress response releases stress hormones into our body, which in turn has a direct effect on the balance of bacteria in our gut. You can clearly see the vicious circle here.
- Diet. Specific diets and foods are known to encourage the growth of good bacteria, preventing dysbiosis and even restoring gut health.
Examples of foods in this category include:- Prebiotic foods (radishes, Jerusalem artichokes, leeks, asparagus, carrots, sweet potato, onions and garlic are all particularly good
- Probiotic foods (fermented foods such as kefir, yoghurt, Kyr, kombucha and fermented vegetables, coconut cheese
- Remove processed sugar and processed foods from your diet. Focus on obtaining natural sugars from fresh vegetables and fruits instead.
- Probiotic therapy can be prescribed for you and is a very effective way of restoring the health of your microbiome. This course of action is likely necessary for long-term emotional health issues.
Written by Annalies Corse BMedSc, BHSc
References:
- Carabotti, M., et al. (2015). The Gut-Brain Axis: Interactions Between Enteric Microbiota, Central and Enteric Nervous Systems. Annals of Gastroenterology. 28(2): 203-209.
- El Aidy, S. et al. (2014). Immune Modulation of the Brain-Gut Microbe Axis. Frontiers in Microbiology. Evolutionary and Genomic Microbiology. April, 2014. Available at: http://journal.frontiersin.org/article/10.3389/fmicb.2014.00146/full
- Monteil-Castro, A. et al. (2103). The Microbiota-Gut-Brain Axis: Neurobehavioural Correlates, Health and Sociality. Frontiers in Integrative Neuroscience. 7: 70. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3791857/
- Reardon, S. (2014). Gut Brain Link Grabs Neuroscientists. Nature. 515: 7526. Available at: http://www.nature.com/news/gut-brain-link-grabs-neuroscientists-1.16316
- Schmidt, C. (2015). Mental Health May Depend on Creatures in the Gut. Scientific American. Available at: http://www.scientificamerican.com/article/mental-health-may-depend-on-creatures-in-the-gut/